Understanding Phlebitis Symptoms: A Complete Guide
Phlebitis, a condition that can affect anyone at any age, involves the inflammation of a vein, often accompanied by a clot. Recognizing the phlebitis symptoms is crucial for timely diagnosis and treatment. Not only can untreated phlebitis lead to further complications, but it also poses significant risks if the veins affected are deep veins in the legs.
What is Phlebitis?
Phlebitis refers to the inflammation of a vein, typically in the legs. There are two primary types of phlebitis:
- superficial phlebitis – affects veins near the surface of the skin.
- deep vein thrombosis (DVT) – concerns veins located deeper within the body.
Recognizing the differences is essential; superficial phlebitis is usually less severe, while DVT can lead to serious complications, including pulmonary embolism.
Common Symptoms of Phlebitis
The phlebitis symptoms can vary based on the severity and type of the condition. However, there are common indicators you should be aware of:
- Pain or tenderness along the affected vein.
- Redness of the skin over the affected area.
- Swelling in the area surrounding the affected vein.
- Warmth in the region where the vein is inflamed.
- Visible veins that appear more prominent or cord-like.
If you experience any of these phlebitis symptoms, it’s wise to seek medical advice promptly.
Causative Factors of Phlebitis
Understanding what causes phlebitis is essential for prevention. Several factors can contribute to the onset of this condition:
- Prolonged immobility—sitting or standing for extended periods, especially during long flights or drives.
- Injury to the vein—any trauma can trigger inflammation.
- Varicose veins—these can strain the veins and lead to inflammation.
- Certain medications, such as those delivered through an intravenous line, can irritate veins.
- Blood clotting disorders can increase the likelihood of developing phlebitis.
Being aware of these risk factors provides individuals a greater chance of preventing the condition from developing.
Diagnosis of Phlebitis
Once symptoms appear, the diagnosis of phlebitis typically involves:
- Physical Examination: The doctor will assess the area for signs of inflammation, tenderness, and other symptoms.
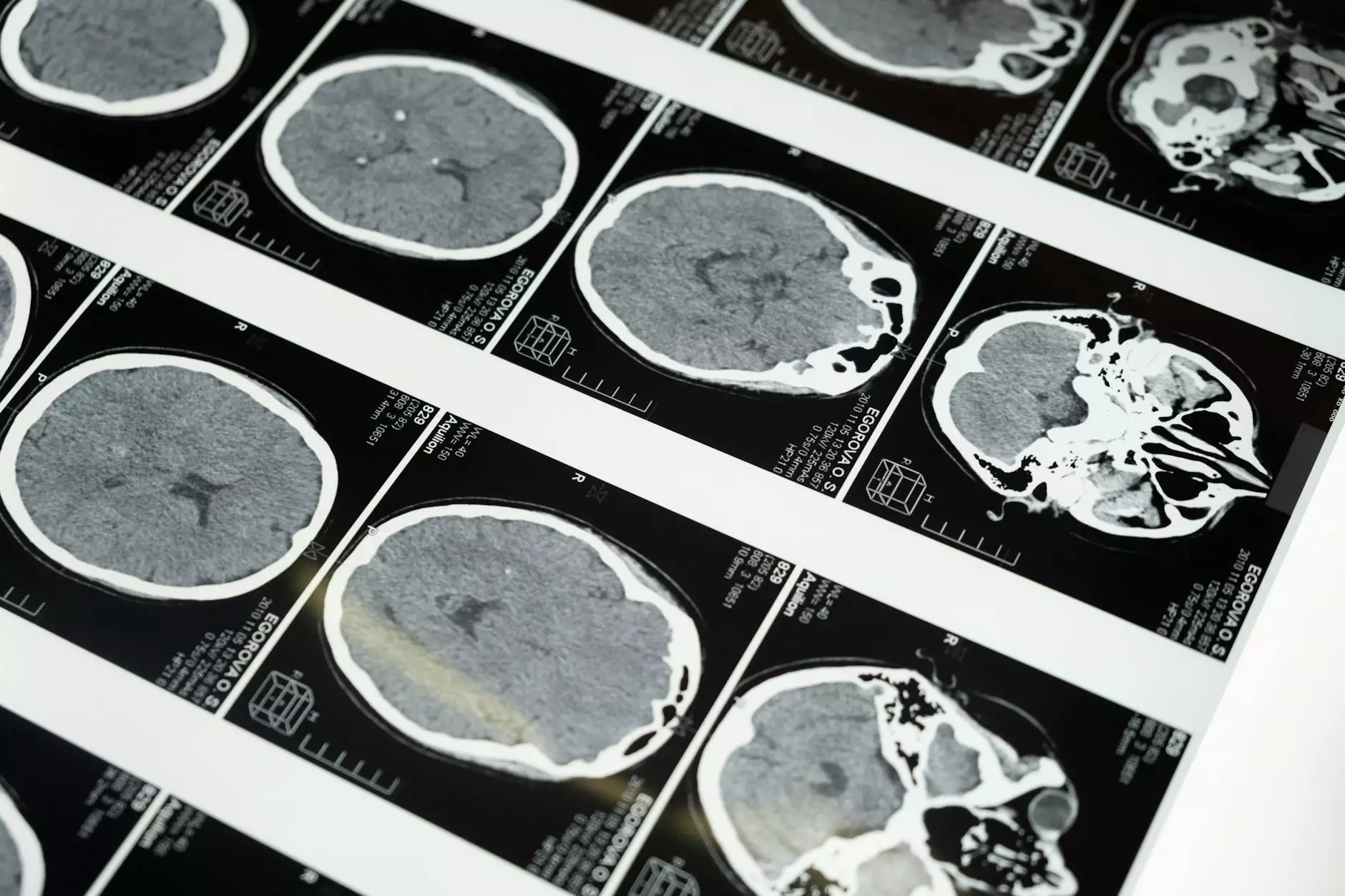
- Ultrasound Imaging: This non-invasive test can identify the presence of a blood clot within the vein.
- Blood Tests: In certain cases, tests may be conducted to check for clotting disorders or infections.
Through these diagnostic steps, a healthcare provider can confirm the presence of phlebitis and evaluate its severity.
Treatment Options for Phlebitis
The management of phlebitis symptoms may vary based on the type (superficial vs. deep) and severity of inflammation. Common treatment approaches include:
- Compression stockings: These can help relieve swelling and discomfort.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Medications such as ibuprofen or naproxen can relieve pain and inflammation.
- Warm compresses: Applying heat to the affected area may help alleviate discomfort.
- Blood thinners: For deep vein thrombosis, anticoagulants may be prescribed to prevent clot growth.
- Procedures: In severe cases, surgical options may be explored to treat clots or damaged veins.
It's essential to follow your healthcare provider's recommendations accurately to ensure proper healing and recovery.
Preventive Measures Against Phlebitis
Preventing phlebitis is crucial for those at risk or who have previously experienced it. Here are some effective strategies:
- Regular movement: Ensure you move around regularly, especially during long periods of sitting or standing.
- Maintain a healthy weight: Excess weight can strain your veins. A balanced diet and regular exercise can help.
- Stay hydrated: Proper hydration aids in overall vascular health.
- Avoid tight clothing: Wearing loose-fitting clothes helps blood circulate more effectively.
- Manage existing conditions: Keep chronic conditions such as diabetes under control as they can contribute to vascular issues.
Implementing these preventive measures could significantly reduce your risk of developing phlebitis.
Living with Phlebitis
For those managing phlebitis symptoms, adopting certain lifestyle modifications can improve their quality of life:
- Engage in regular exercise: Low-impact activities like walking or swimming can help promote circulation.
- Apply skin care: Keeping the skin clean and moisturized may aid in reducing irritation.
- Follow medical advice: Regular check-ups with a healthcare provider can help track your condition over time.
- Educate yourself: Understanding your condition can empower you to take control of your health.
Staying informed and proactive is vital for anyone dealing with this condition.
When to Seek Medical Help
Although many cases of phlebitis can be treated effectively with self-care and medication, certain situations warrant immediate medical attention. Seek help if you notice:
- Sudden swelling or intense pain in the affected limb.
- Fever or other signs of infection.
- Shortness of breath or chest pain, which may indicate a pulmonary embolism.
Your health should always be your top priority, and recognizing when to act provides the best chances for a good outcome.
Conclusion
Understanding and recognizing the phlebitis symptoms is essential for anyone who may be at risk. Early diagnosis and appropriate treatment can prevent serious complications and improve one’s quality of life. At Truffles Vein Specialists, our team of experts in vascular medicine is dedicated to providing comprehensive care for individuals dealing with phlebitis and related conditions.
If you or someone you know is experiencing phlebitis symptoms, don’t hesitate to contact us for a consultation. Your health is paramount, and our professionals are equipped to guide you every step of the way.



